Abstract
Background: Prior studies have demonstrated disparities in the utilization of stem cell transplant (SCT) based on age, race, and insurance type. Whether delays to SCT occur as a result of these disparities is not well established. We evaluated whether we observed similar trends in a large metropolitan SCT center with a large population of minority patients (pts).
Methods: We identified pts at Karmanos Cancer Institute who had their initial SCT consultation from 2009 - 2016, and evaluated pts who received or did not receive SCT for the diagnoses of acute myeloid leukemia (AML), acute lymphocytic leukemia (ALL), myelodysplastic syndrome (MDS), multiple myeloma (MM), or non-Hodgkin lymphoma (NHL). The associations of SCT receipt status with 4 chosen predictors (age at the initial SCT consult (continuous variable), race [Caucasian vs. Non-Caucasian], sex, diagnosis [AML/ALL vs MDS vs. NHL vs MM]) were assessed by logistic regression models. Of those who received SCT, time to SCT was calculated from the date of coordinator intake (date of 1st SCT consult + screening initiated) to the date of SCT. Kaplan-Meier estimates were used to summarize the distributions of time to SCT. Cox proportional hazards regression models were fit to assess associations between 7 prespecified predictors (age, race, sex, diagnosis, type of SCT [Auto vs. Allo], county [Metro (three counties within Metro Detroit) vs. Non-Metro], and insurance [Private vs. Public (Medicaid, Medicare, others)] and time to SCT.
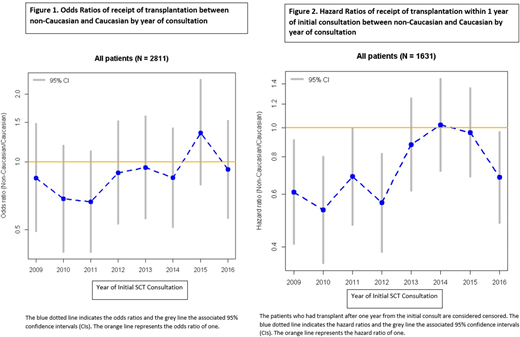
Results: 2811 pts were included in our study, and of these 1644 received SCT. In multivariable analyses, non-Caucasian (n= 585 with 495 African-Americans) compared to Caucasian (n=2226) (OR 0.68, p<0.001, 95% CI 0.56-0.83), and NHL pts (n=750) compared to MM (n=1136) (OR 0.38, p<0.01, 95% CI 0.31-0.46) or AML/ALL(n=642) (OR 0.76, p=0.01, 95% CI 0.61-0.95) and older pts compared to younger (OR 0.97, p<0.001, 95% CI 0.97-0.98) were less likely to receive a SCT. There was an interaction of race with both age and diagnosis; therefore propensity match scoring analysis was performed to reduce selection bias due to these interactions (matching Caucasians and non-Caucasians by age and diagnosis), resulting in 1170 matched pts. Multivariable analysis among matched pts revealed that older compared to younger, non-Caucasian compared to Caucasian, and NHL pts compared to MM pts were less likely to receive SCT and remained independently significant. Interestingly, these differences in ORs of SCT between non-Caucasians and Caucasians depended on the year of initial consultation, and diminished over time (Fig 1).
We then evaluated all pts who received SCT (n=1631). 1307 (80%) were Caucasian and 324 (20%) were non-Caucasian (273 were African-Americans). The median time to SCT was 3.24 months for all pts and 75% underwent transplantation by ~4.5 months. In the multivariable analysis, non-Caucasian (median 3.8 months) compared to Caucasian (median 3.28 months) (HR 0.75, p<0.01, 95% CI 0.65-0.85), public insurance (n=800, median 3.43 months) compared to private insurance (n=831, median 3.28 months) (HR 0.90, p=0.04, 95% CI 0.81-0.99), auto SCT (n= 983, median 3.51 months) compared to allo SCT (n= 648, median 3.1 months) (HR 0.82, p<0.05, 95% CI 0.67-0.99), and NHL pts (n=360, median 3.57 months) compared to AML/ALL pts (n=367, median 2.95 months) (HR 0.74, p<0.01, 95% CI 0.61-0.90) had significantly longer times to SCT. To reduce selection bias due to the association of race with age, county, type of SCT, insurance, and diagnosis, propensity matched scoring analysis was performed between races resulting in 624 matched pts. After matching, multivariable analysis still demonstrated that non-Caucasian and public insurance were independent factors in delay to SCT. However, differences in HRs of time to SCT between races depended on the year of consultation and improved over time (Fig 2).
Conclusion: In this large retrospective analysis, we observed that race, age, and diagnosis are independent significant factors impacting receipt of SCT. Race and insurance status were independent factors associated with more prolonged time to SCT. Importantly, the effect of racial disparities in receipt of SCT and time to SCT are declining over time. Further analysis of the impact of social, medical, and financial factors are in progress.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal